The experience of a hypnotic trance not so unusual or strange. To the contrary, it feels vaguely familiar to countless other moments in your life where you were absorbed in a zone, lost in thought, enthralled by bliss, or perhaps simply meditating.
Meditation is actually the closest you can come to a state of trance without being guided there, as you would experience in hypnosis. I often refer to it as taking my clients on a journey, a metaphorical trip in your mind or imagination.
There are countless ways to enter a trance. It is similar to falling asleep just not losing conscious awareness. That means that you are able to hear and sense things around you but, typically your eyes are closed, you are not moving, just resting comfortably relaxed. Amazing things happen when you relax on purpose. You should notice that your breathing slows down and most of your muscles become relaxed. There is this sense of distance from where you are, the passage of time gets distorted and often you feel a pleasant, almost euphoric state of peace.
The depth of a hypnotic trance varies, it can be very light or extremely deep. When you feel comfortable with the hypnotherapist, you are willing to “let go” to and allow yourself to enter a trance, then you can experience the special power of the mind and imagination. The power of hypnosis does not depend on the depth of the trance, rather it is a matter of skills the hypnotist has to help you experience something special.
As you enter hypnosis, you actually disconnect your mind from the body and surroundings. That means that your awareness is withdrawn from the normal alert state you walk around in and goes inwardly. The power of hypnosis is your ability to harness the full potential of your imagination without the normal restrictions of the critical mind. This is when a skilled hypnotherapist can help you make dramatic changes in your life. The hidden power of trance is in the suggestions you listen to and how much you embrace these new ideas.
Hypnosis does feel very nice and relaxing, almost like taking a nap. The big difference is in what you are guided to experience during the trance. There are many unusual effects that hypnosis can have on a person. An example of a famous one is the arm levitation, where your arm rises up with a distinct sense that you are not doing it intentionally.
There are many strange sensations a person can have during a trance which can only happen under hypnosis; none of these can cause you any harm or pain. Remember, that you cannot be hypnotized against your will, it works only if you agree to let it happen. So, perhaps you are now getting a bit more curious about taking a journey and exploring the hidden labyrinth of your mind.
By: John Ryder Ph.D. Psychology Today
This video highlights benefit of hypnosis for a woman who needed breast surgery.
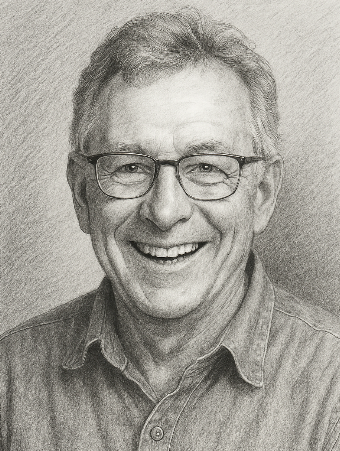
Thanks for sharing your story with us Paul. So, let’s start at the beginning and we can move on from there.
After working for 10 years at Massachusetts General Hospital and in homecare Hospice as a Registered Nurse, I was ready for a change and wanted to pursue self-employment. I was interested holistic modalities and had used Hypnosis for my own public speaking phobia while in college, and it worked great.
After leaving nursing, I spent 3 months searching for the right path and when someone mentioned Hypnotherapy as a possibility, it caught my attention. After taking my first certification course I instantly had a good feeling about it.
I opened my practice, ‘Burlington Hypnosis’, in October of 2001. Soon I was fortunate to appear on Boston radio, WBZ 1030AM, which soon led to an appearance on WCVB TV’s ‘Chronicle’. My practice quickly grew and in 2007 I started hosting my own cable TV show ‘Healthy Hypnosis’ which I marketed to 25 Greater Boston communities.
My medical background as a Registered Nurse sets me apart from most of my colleagues, especially when working with clients who have medically based difficulties. I better understand their situations and can use Hypnotherapy to help them find relief.
We’re always bombarded by how great it is to pursue your passion, etc – but we’ve spoken with enough people to know that it’s not always easy. Overall, would you say things have been easy for you?
Being self-employed in any field is challenging and at times overwhelming. In spite of such a quick start to my new practice, I was still trying to make a living in one of the most misunderstood, disregarded fields there is.
Initially, I thought I would easily get referrals from the mainstream medical community because of my medical background, but this was not the case. New England has very deep, old-school roots, so getting my foot in that door never really happened the way I thought it would.
Another challenge involved the craft itself. In order to generate word of mouth referrals, I needed to be good. Becoming a confidently, effective Hypnotherapist took time and practice. So I offered free sessions, spoke to any group that would have me, and slowly established my hypnotic comfort zone.
Thankfully I made a few friends in the field over the years and we often compare notes, techniques and share frustrations which has been a big help to all of us over the years.
Times got so tough I even tried to leave the field a few times, but I always came back. Being able to help people in need with Hypnotherapy is an incredibly fulfilling experience. I am so grateful to have stumbled into this profession and stuck with it as long as I have.
So let’s switch gears a bit and go into the Burlington Hypnosis story. Tell us more about the business.
I am a sole proprietor in every sense of the word. I am directly involved in web design and optimization; social media and marketing; producing my TV show and editing video as well as writing and recording a wide array of Hypnotherapy programs covering most of the typical day-to-day problems that people struggle with.
I see many clients dealing with a wide array of stress/fear related problems including exam performance, fear of flying and public speaking. I also see many struggling with chronic generalized anxiety, confidence issues, and even depression.
My medical background serves me well-helping individuals with peripheral neuropathy pain, irritable bowel syndrome, tinnitus, and substance abuse. Hypnotherapy enhances the mind-body connection which can offer relief in ways one might not ever expect.
The program I am most proud of is my Virtual Gastric Band weight loss program. This unique approach guides individuals to imagine that they have undergone a medical procedure to ensure weight loss. Initially, I was reluctant to get into this application because I have always been against the real-life surgical approach, but I quickly learned how effective it is. I routinely have clients reporting more than 40-pound weight loss and have many video testimonials posted on my site.
What sets me apart from many of my colleagues is not only my medical experience in general but specifically my work in homecare Hospice. It was important to gain trust and develop a rapport with these patients and their families, and the best way achieve this is to simply listen. The art of listening is very therapeutic for patients in Hospice as well as with my Hypnotherapy clients.
Has luck played a meaningful role in your life and business?
I was lucky in so many ways throughout my 16-year career as a Hypnotherapist, starting with the uniquely unexpected conversation with a local practitioner, who first mentioned the field of Hypnotherapy. I saw her ad in the local paper about her Reiki practice so I called. She took the time to speak with me about holistic modalities and she also put me in touch with my first Hypnosis instructor.
I was also lucky when discussing this option with my wife. If she hesitated at all I probably would never have taken this path. Thankfully there was no hesitation; she instantly said that if I thought it felt right I should proceed.
Luck was also in my corner when one of my very crude brochures landed on the desk of Paul Sullivan at WBZ radio. He hosted a nightly talk show and thought I would make an interesting guest to interview. This lucky connection began a 15-year relationship with WBZ. Unfortunately, Paul passed away in 2007. His replacement Dan Rea said that ‘if I was good enough for Sully I was good enough for him.’ I have been on with Dan twice/year since.
Luck continued to carry me when I sent an audio CD of my first WBZ appearance to WCVB-TV and was soon contacted to appear on an episode of ‘Chronicle’ dedicated to Hypnosis.
I was certainly desperate to make this new career track happen, and looking back it seems as though the universe was right there guiding me every step of the way. I got to continue making important connections with people in need and don’t feel like I’ve worked a single day yet.
[Article post]
Well done video produced by ‘The Factoid’ on how hypnosis works.
It sounds like the work of sorcerers and scam artists, but hypnosis can play a very real role in protecting and promoting health. This isn’t the “You are getting very sleepy…” hypnosis you’re used to seeing in pop culture references, but a clinical procedure used in conjunction with other therapies and treatments, according to the American Psychological Association.
Hypnosis for health benefits “should be conducted only by properly trained and credentialed healthcare professionals (e.g. psychologists) who also have been trained in the use of hypnosis and who are working within the limits of their professional expertise,” according to the APA’s website.
The “state of inner absorption, concentration and focused attention” brought on by hypnosis may help us use our minds more powerfully, according to the American Society of Clinical Hypnosis (ASCH). And harnessing the powers of the mind has inspired researchers and clinicians in various fields to explore the use of hypnosis in a number of health outcomes.
Medical hypnosis, sometimes called hypnotherapy, uses verbal repetition and/or mental imagery (facilitated by a hypnotherapist or one’s self) to induce a “trance-like state” of increased focus. It’s typically described as feeling calm and relaxing and usually opens people up to the power of suggestion, according to the Mayo Clinic.
Once disregarded as a parlor trick, hypnosis is increasingly believed to improve many of those outcomes. The American Medical Association approved hypnosis as a therapy in 1958 (although it later rescinded its position, according to the ASCH), and the APA followed suit three years later, according to Harvard Medical School.
That’s not to say it’s a panacea: In fact, more research is needed to prove lasting benefits of hypnosis for certain facets of health, such as weight loss or smoking cessation. But more promisingresults exist in other areas of study. Here are a few of the science-backed benefits of hypnosis to consider.
Hypnosis can help improve deep sleep.
In previous studies of the effects of hypnosis on sleep, study participants were simply asked to report back on how well (or poorly!) they felt they slept after hypnosis. But in a recent study, Swiss researchers were able to measure its effects by monitoring brain activity in a group of healthy, young women as they took a 90-minute nap after listening to a hypnotic suggestion tape.
The women who were deemed the most susceptible to hypnosis spent 80 percent more time in slow-wave sleep (the deep, restorative phase of our shut-eye) after listening to the hypnosis tape than they did after listening to a neutral spoken text. “The results problems and for older adults,” lead researcher Maren Cordi of the University of Zurich said in a statement. “In contrast to many sleep-inducing drugs, hypnosis has no adverse side effects.”
It can ease symptoms of irritable bowel syndrome.
In a 2003 study, 71 percent of 204 irritable bowel syndrome (IBS) patients reported improved symptoms after 12 weekly hour-long hypnosis sessions, the APA reported. Of those who reported improvements, 81 percent continued to feel better up to six years after the hypnosis treatment had ended, according to the study.
In a 2012 study, 85 percent of IBS patients who reported improvement after hypnosis still felt better up to seven years later. “The conclusion is that hypnotherapy could reduce both the consumption of healthcare and the cost to society and that hypnosis, therefore, belongs in the arsenal of treatments for IBS,” researcher Magnus Simrén said in a statement.
Hypnosis can quell hot flashes
Among postmenopausal women who reported at least 50 hot flashes a week, five weekly hypnosis sessions cut hot flashes by 74 percent 12 weeks later, a 2013 study found. Meanwhile, women who did not receive hypnosis but instead had weekly sessions with a clinician only experienced a 17 percent drop in hot flashes.
It can ease pain
Hypnosis is perhaps most well-researched in the context of managing pain. Two meta-analyses of existing pain and hypnosis research, published in 2000 and 2009, deemed hypnosis effective at lowering pain associated with a number of conditions, including fibromyalgia, arthritis, and cancer, but noted that few psychologists were using it, and those who were had little standardization in administering hypnotherapy.
Hypnosis can calm nerves
Because of its ability to harness the powers of the mind, hypnosis is often employed to relieve anxieties related to other medical procedures, like surgery, scans or even giving birth, called state anxiety. “The mechanism may be similar to the placebo effect — in which patients’ expectations play a major role in how they feel,”
Melinda Beck wrote for the Wall Street Journal in 2012. “Hypnosis, in turn, can help patients adjust those expectations to minimize pain, fear, and disability.” More research is needed to determine if hypnosis might alleviate generalized anxiety disorder or what’s called trait anxiety, or anxiety relating to personality rather than a specific event, according to a 2010 review of the research. Preliminary studies have started to examine hypnosis in depression treatment as well, but more research is needed.
By: Sarah Klein